The science behind panic attacks — and what you can do to manage them
Have you ever woken up in the morning — or even in the middle of the night — only to find that your body is already in full-blown, heart-racing fight-or-flight mode?
Panic attacks are surprisingly common; at least one-third of us will experience one at some point in our lives, according to Cindy Aaronson PhD, a clinical psychiatrist at Mount Sinai Health System in New York City. While symptoms vary from person to person, they can include a pounding heart, shortness of breath, light-headedness, sweating, trembling, nausea, tingling or numbness in the fingers and toes, and an overwhelming sense of impending doom.
Despite how terrifying and memorable panic attacks can be, they are not inherently dangerous.
For many people, these alarming sensations — which can mimic those of a heart attack or other serious medical condition — are accompanied by a conviction that they are about to die. For others, says Aaronson, there’s a sensation of “unreality,” where time and perception become scrambled. “Sounds sound different — you feel like you’re in a tunnel and things are far away; colors seem different. People sometimes describe it as an out-of-body experience,” she says. “They feel like they’re going to lose control and go crazy.”
It’s no surprise, then, that many people in the grips of a panic attack show up at the emergency room believing that they are having a heart attack or suffocating. But despite how terrifying and memorable these episodes can be, they are not inherently dangerous, says Justin Feinstein PhD, a clinical neuropsychologist and director of the Float Clinic and Research Center at the Laureate Institute for Brain Research in Tulsa, Oklahoma.
Instead, panic attacks are a manifestation of the brain and body being out of sync, he explains.“It’s a normal physiological fear response happening at a totally inappropriate time.”
Here’s what happens in your body during a panic attack
Even though psychiatrists have been investigating just what panic is since the mid-to-late 1800s, the term “panic disorder” didn’t appear in the Diagnostic and Statistical Manual of Mental Disorders until 1980. Experts still aren’t sure precisely what underlies this disordered brain-body connection.
“Sometimes panic might start in your body itself, and then create processes within your brain. Other times, your brain could initiate the entire onset of a panic attack, which then manifests itself in your body,” says Feinstein. In some cases, genetics or changes in brain function may be at play. In others, stress is a factor.
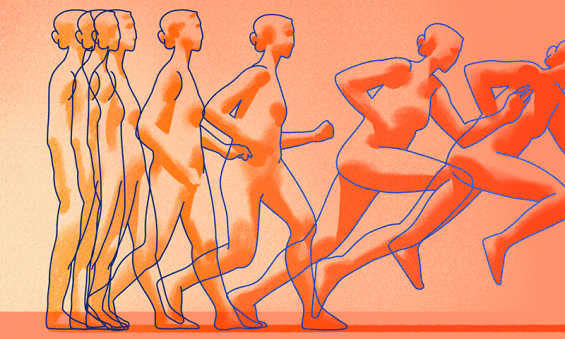
Panic attacks begin with something that causes your heart to race — it could even be caused by something as innocuous as a jolt of caffeine.
But once an attack is triggered, the cascade of physiological responses in the body is fairly universal. Typically, it begins with something that causes your heart to race. This might be a stimulus in the environment — perhaps a sound or a scent that you associate with a traumatic event — or even something as innocuous as a jolt of caffeine. In a panic attack, the racing heart sets off a danger alarm in your brain and sends your body’s fear response into overdrive.
Your amygdala — a pair of almond-sized nerve bundles buried in the deep brain that plays a key role in processing emotions — sends a distress signal to your hypothalamus — a tiny command center that sits atop the brainstem and coordinates involuntary bodily functions such as breathing, blood pressure and heartbeat. Your hypothalamus fires messages via the autonomic nervous system to the adrenal glands, prompting them to flood your bloodstream with hormones including adrenaline and cortisol. These chemical messengers engage your body’s survival reflexes and ready it to take defensive action.
Your pupils dilate, and your mind becomes laser focused. Your breathing rate increases, allowing your body to take in extra oxygen. Cellular metabolism shifts to maximize the amount of glucose available to the brain and muscles. Your blood is diverted away from non-essential regions like your fingers, toes and stomach and towards the major muscles of the arms and legs — steeling them to either fight off a threat or flee the scene.
Panic attacks typically peak and subside within 10 or 15 minutes, and there are a handful of solid techniques that can help you ride them out.
That, in a nutshell, captures the traditional scientific thinking about panic attack. “The amygdala has always sort of been viewed as the fear epicenter,” says Feinstein.
However, recent work from his lab suggests that other structures in the deep brain may also be involved. Specifically, the insular cortex and a part of the brain stem called the “nucleus of the solitary tract” — regions that together receive and map signals from the heart, lungs and bloodstream. Feinstein’s team found that these areas generate fear impulses even in people who have been missing an amygdala due to a rare brain injury, suggesting that panic may often begin here in other people, too.
So, how can we hit the brakes?
To be classed as a panic attack, symptoms must come on rapidly, or within a few minutes, says Aaronson. And there’s good news: Attacks typically peak and subside within 10 or 15 minutes, and there are a handful of solid techniques that can help you ride them out.
Chief among those is recognizing your experience as a panic attack and not a more serious medical crisis, and gently reminding yourself that there’s nothing physically unsafe about it. “Just knowing what it is helps people,” says Aaronson. Just to be sure, double-check that you’re not experiencing any heart-attack specific symptoms such as pressure in the chest or pain that builds or radiates into the arm or jaw.
Once you’ve ruled those out, remember: Panic always passes, and focusing on that belief can send it on its way.
Of course, this is easier said than done when you feel like you’re suffocating or losing control. “It takes practice,” says Aaronson. “But the more you do it, the better you get at doing it.”
You might tell yourself: “Everything my body is doing right now is designed to keep me safe and protect me.”
If you can, find a quiet spot where you can talk yourself through why you’re feeling what you’re feeling.
For example, you might tell yourself: “I’m feeling light-headed because my blood is being redirected to my limbs. I’m breathing hard because my body is responding in an evolutionarily honed way to adrenaline. Everything my body is doing right now is designed to keep me safe and protect me.”
When you do this, you’re inviting another region of the brain into the conversation — the frontal cortex. This area is positioned just behind the forehead, which is responsible for conscious thought, judgement and problem solving. Bringing a sense of curiosity and analysis to the way you observe these sensations can help you to underline that they are just transient physical processes moving through you.
The other major tool in your toolbox is your breath. “Most people breathe on average from 12 to 20 breaths a minute. And when you’re hyperventilating, you’re easily doubling that,” says Feinstein.
He recommends trying to gradually slow your breathing to between five and 10 breaths per minute, and aiming to make your exhales longer than your inhales. This simple technique engages a parasympathetic response — fight-or-flight’s calming cousin, also referred to as “rest-and-digest.” Try doing this simple exercise from Judson Brewer, psychiatrist, neuroscientist and director of research and innovation at Brown University’s Mindfulness Center in Providence, Rhode Island.
This kind of deep breathing stimulates the vagus nerve — the longest nerve in the body, which runs through regions including the digestive system and diaphragm, and feeds directly into the brainstem’s nucleus of the solitary tract. It carries signals and sensory information from and to the brain, and regulates functions including heart rate, breathing rate and digestion.
“Ultimately, panic attacks are just fear of fear,” says clinical psychiatrist Cindy Aaronson, PhD.
Interestingly, your vagus nerve is a two-way street. By breathing in a slow, controlled manner, you send a powerful signal to your brain that you are relaxed and there is nothing to fear. In turn, this stimulates certain parts of the heart muscle and helps to steady the pulse.
When practiced regularly, longer-term practices such as mindfulness meditation, which are usually built around a core of breathing techniques, can help people quash attacks before they take hold, says Feinstein. “[Mindfulness] teaches people a new association with their visceral experiences,” he explains. Focusing intently on your breath and heartbeat in a relaxed setting can help you shake off any reflexive jump to panic when they speed up in everyday life.
Therapy can help too. Aaronson’s group found that cognitive behavioral therapy, which is designed to gradually help you modify your behavioral responses to life events, can strengthen the neural connections between the frontal cortex and the amygdala. This makes panic sufferers more adept at talking themselves down off the ledge.
“Ultimately, panic attacks are just fear of fear,” says Aaronson. In the US alone, at least 1 in 10 Americans experiences a panic attack in any given year — the same number as fall ill during a bad flu season — so if you find yourself having one, know that you have plenty of company.
And just as your body responds to the flu virus by igniting a fever, it can sometimes respond to fear by firing up a panic attack. But with a little help and a few key techniques in your arsenal, you can take the wind out of panic’s sails. “If [you’re] not afraid of it, then who cares if it happens?” says Aaronson. “It passes.”
Watch Dr. Aaronson’s TED-Ed Animation on panic attacks now:
ABOUT THE AUTHOR
Ceri Perkins is an NYC-based writer and editor who covers the environment, science, nature and human behavior. Her work appears in BBC Earth, Physics World, The Guardian, How it Works and more. Find her on Twitter @pepperjayperk.
This piece was adapted for TED-Ed from this Ideas article.